A few weeks ago at the ADI2017 conference in Kyoto, DAI and DAAT member John Quinn gave a great presentation We Need to 'Think Outside the Box", especially in relation to rehabilitation enablement and dementia. Thank you John for allowing us to showcase it here.
His power point slides can be downloaded here We need to ‘Think Outside of the Box ’_John Quinn_ADI Kyoto2017 and his full speech notes are below:
"A friend of mine was diagnosed with Fronto-Temporal Dementia. He used to be a truck driver and tinkered with cars and engines most of his life. But only 18 hours after he had MRIs etc that resulted in his diagnosis, he lost his licence. He felt that his whole life had shattered. At the time, he was in his mid 40s, with four children. His wife had to return to full time work to continue paying off the mortgage and to support the family. But by the time he was 50 years old, when his youngest child was 7 years old, he was placed into a Care Facility, because there was no one at home to care for him. The average age of the other residents was about 85 years old. He felt hopelessness… and also a failure, because he couldn’t provide for his family.
There was no immediate rehabilitation for him, however; soon afterwards, his friend told him about a group of men who were rebuilding an antique truck. Years later, they still catch-up every week to work on this project together. Now he is proud of what he is achieving albeit small steps. In time, the organisers hope that there’ll be a restored, functioning, antique truck available for street parades, TV advertisements and movie sets.
This is an example of what rehabilitation might look like. OR is it enablement? OR… is it empowerment?
In some health areas, for example with various forms of addiction, the word enablement has different connotations than in the Dementia arena, so we must be mindful of the meaning of words here, too. Also, I’ll later refer to how I felt disempowered by others, then later with time and unexpected support, regained the sense of feeling empowered. Some of us who live with Dementia are advocating for the correct use of language in the media and within our Communities. Perhaps here is another area where better awareness of language can improve our lives. Whatever the correct word is, the result should be better outcomes for people living with Dementia. Here in this context, for simplicity, I’ll use Rehabilitation and Engagement interchangeably. However, it will only be effective if it empowers us.
In an ideal world, some types of rehabilitation relevant to the person’s current life and the personal symptoms of Dementia should be offered at the time of diagnosis. Everyone has a Right to Rehabilitation to his or her changing abilities, BUT let’s not dismiss ANY type of rehabilitation. We need to ‘Think Outside of the Box”, for the best outcomes to empower us. Everything with value will be valuable!! Who determines what is valued? I believe that it must be the person with the diagnosis in the first instance. This type of conversation and the ensuing negotiation is relevant regardless of the age of the person living with Dementia.
However, it is more important when someone young is diagnosed, as there is an emerging realisation that when a younger person is diagnosed with Dementia at the earliest opportunity, there will be a longer period of successful engagement with his or her current lives. Immediate support and contact with someone who can guide the person living with Dementia and their family through this tumultuous life-changing period, would maintain some hope for the possibilities for the future; and, feelings of being valued as a person who can still contribute to their family and society.
At least in my own case, I believe that I still could have had a sense of purpose and self esteem… But I lost them when I lost my career. The career that I loved and was respected in, had taught me skills and knowledge for 35 years. Yet suddenly, in 2008, I not only couldn't do it due to my symptoms, I didn't have the opportunity to return to it with support or adaptations post diagnosis.
Interestingly, for the past two years, with encouragement and lots of support, I’ve been able to use those skills that I learnt throughout my lifetime in my career… in my advocacy. This advocacy has also opened many new pathways and opportunities for me, that I couldn’t have envisaged, and I value that. Through my advocacy, I've met new, genuine lifelong friends; I’ve had the opportunity to meet with people who inspire many; and I’ve been to places that I wouldn't have considered before. I've regained a passion, a focus and a purpose again. Prior to this, I’d felt that everything about who I was, had been taken away from me…..by Dementia, and by the responses of those who could have offered support if they’d only looked at me as the person who I was…………not just as Dementia.
I can’t learn new things easily. I get lost in the process and if I do manage to learn new things, it takes an enormous amount of time and effort on my part, and patience by others. However, I still had, and still have, many skills and expertise in particular areas that the post-diagnostic model forgot to address or encourage. In my case I was an educator…..a School Principal or Deputy Principal of large Primary Schools. Therefore, I spent my adult life in education, learning new things and mentoring others; encouraging both the students and fellow educators to engage in learning skills and knowledge for a successful life. In other words, life long learning
But who else was I? What else was I passionate about?
I’ve always been a caring person and a family man.
But also, what comes to mind is my interest in active participation in sports. I not only trained and encouraged the students in a number of sports, at the school that I was at, but I also enjoy being a spectator of many sports.
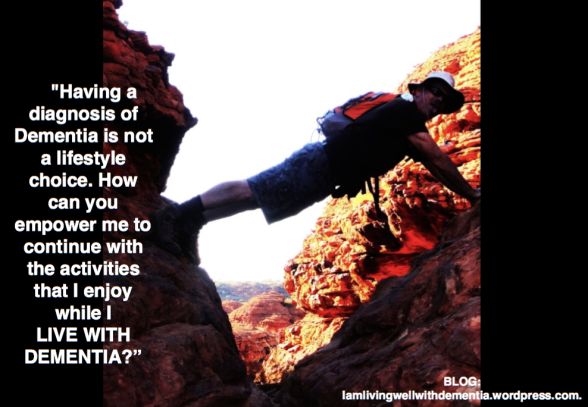
During the last 25 years, I’ve run 3 marathons, about 20 half-marathons, a triathlon, and 30 charity fun runs, so as you can imagine I’ve always been reasonably fit. However, I have also participated in many challenging feats in recent years since my diagnosis, such as the Great Wall of China half-marathon, and climbed Mt Taranaki in New Zealand. In addition, since I started being involved with advocacy, I’ve also used my athletic ability to raise much needed funds and awareness in 2 separate challenges…..cycling through Vietnam and Cambodia after buying a bike when I couldn't drive any longer; and walked our second Camino de Santiago, 825 kms from France across the top of Spain. Whist I could do the physical challenges they wouldn’t have been possible without the support of others, particularly my partner Glenys who did the planning, organisation and problem solving to ensue that I was able to successfully undertake these events.
So each one of us already had expertise, interests, and passions prior to our diagnosis, which if acknowledged and carefully nurtured and encouraged, can enable us to remain independent and interested in engaging in our future lives, albeit with some adaptations and support where necessary.
We need to look beyond the deficit model of what we can’t do, and instead look at the skills and knowledge that we already have. Board-certified Internist and Geriatrician, Dr Allen Power agrees…In his book ‘Dementia Beyonds Drugs’, he states…“Although there are cognitive deficits, many complex abilities are already preserved, which should be identified and cultivated”…..Others in the medical field; allied health professionals; Governments and organisations; and, our family and friends, need to get on board with this concept to encourage us to maintain our skills; and, provide individualised personal programs and career support, so that we can continue to be independent for as long as possible.
I already know what I can’t do. I knew about them years before I received an accurate diagnosis. I’m reminded of them daily when I get confused or frustrated, knowing that everyone is thinking at a different speed and level. I am particularly reminded of them, when I travel; have the rare late night with my son at the football; or, after the many social interactions that occur throughout each day. And strangely, I’m subtly reminded of them when some people challenge my diagnosis, because I can interact with others and I’m reasonably fit, therefore don’t look like I have Dementia. However, they don't see how I can’t function for hours, after engaging in most activities.
Please don't misunderstand me though. The type of rehabilitation that people usually think of, is also very important, for example, Occupational Therapy, Speech Therapy, Physiotherapy. However, when it’s Dementia, aren’t these therapies really enablement? I’m never going to rehabilitate back to close to my former self, as I may have after a stroke or heart attack.
In about 2011, after my diagnosis, Glenys said to my neurologist that she was aware that there are Speech Therapists who specialise in rehabilitation after a Heart attack or Stroke. She questioned whether there was one who specialised in Dementia, to hopefully provide some strategies and knowledge that we didn’t have, that might assist us in our daily communication……His reply was that he'd never been asked that question before.
There have been some changes though. This time last year, we were asked to give the Consumer Perspective to the Australian Federal Minister for Health on a new government document for People with Dementia. This document has some excellent points enmeshed in the 109 ‘Principles of Care’.
There are two references to accessing Speech Therapists…..But we also need speech/language therapy for people who have word finding, processing problems, or other language concerns etc, like I have?
The medical profession needs to consider authentic rehabilitation which is vital for younger people living with dementia or those early in the dementia process. Are some attitudes because dementia is a terminal condition for which there is no cure? I don’t know…..However, through my involvement on a national committee where up to 40 different research activities are currently happening, I’m aware that there’s some good, innovative research that includes a focus on empowerment. So there’s emerging hope for a change in attitudes.
I have personally done a little research on what can impact on the progression of Dementia and what keeps our brains healthier…..things like the effects of music; and learning new languages and skills. As a result I’ve formed an acronym….It’s my N.A.M.E.S……names….N for Nutrition; A for Attitude and Acceptance; M for Mental activities, Music and Meditation; E for Exercise and Enjoyment; and S for Support, Sleep, Socialisation, and Setting Goals. Some of the activities that I engage in for my NAMES, include, learning Spanish; doing crosswords with my non-dominant hand; volunteering each week; advocating; writing to the Editor of the local newspaper; and, writing a blog. My N.A.M.E.S. keeps me on track to do what I believe will help me.
I want you to consider these questions. What value do our existing skills hold? What value is there in learning through experience rather than in isolation, for example, in a one-on-one class with a therapist? What value do we place on participation with fun, social engagement? How can we be empowered through support and opportunity to live as independently and as fulfilling a life as possible? I’ll finish with another quote by Dr Allen Power, in “Dementia Beyond Drugs”. Well-being is not dependent on cognitive and functional ability and should be maximised in all people. There has to be a paradigm shift in the way we view people with Dementia
Thank you."